"It's a tough time in health care, and our clinicians and systems are struggling. We need to take a deep breath and go back to the science to effect change together."

Berwick
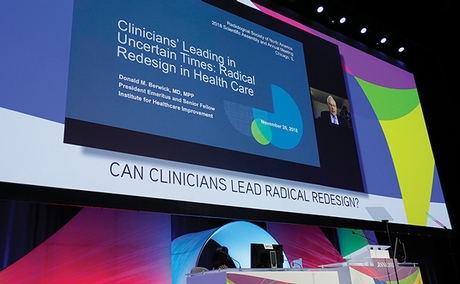
This was the overarching message in the Monday plenary session delivered remotely by Donald Berwick, MD, MPP, president emeritus and senior fellow of the Institute for Healthcare Improvement in Boston.
Dr. Berwick presented an historical examination of the state of the medical profession exploring the reasons former and current practices are inadequate for delivering the type of health care patients demand and that physicians strive to provide.
"Years ago, medical professionals had a social contract that assumed a nobility in the profession. The understanding was that when something went wrong, the profession would take care of the problem. This was a hero's approach," Dr. Berwick said.
He noted, however, that in the second half of the 20th Century, studies revealed an appalling number of avoidable errors and lapses in health care.
"The response to the gap between what medical professionals were doing versus what could be done brought about a new era in which additional scrutiny was applied and payment incentives were attached to performance. This was war on the profession," Dr. Berwick said.
Scrutiny and value incentives did not improve health care and, more likely, were demoralizing to doctors. Instead, Dr. Berwick recommended a model known as the "Triple Aim" of health care.
"We must provide better care for individuals, better health for populations and lower per capita cost through improvement. Only redesign will get us there," he said.
The principles of the radical redesign outlined by Dr. Berwick are: Change the balance of power, standardize what makes sense, customize to the individual, promote well-being, create joy in work, make it easy, move knowledge — not people, collaborate/cooperate, assume abundance and return the money.
"Clinicians can take the lead in bringing these design concepts to reality by remaining open to new ideas," he said.
Dr. Berwick shared an example of the principle of changing the balance of power through the story of the remarkable success experienced at an institution in Sweden where, inspired by one of their patients, physicians began allowing patient-administered, self-care dialysis.
The patient later encouraged the practice at another institution in Waco, Texas. Patient involvement created a radical change in their attitudes and outlooks as well as in staff responsibility. Staff become teachers, coaches and trainers who share the power in delivering necessary care.
"Historically we worked our way into a bit of a mess," Dr. Berwick said. "Trained as proud professionals, if we stay in our channels and we're taught to be heroes, we begin to lose sight of the system. Likewise, the rewards, punishment and payment incentives do not work because they do not produce change. There is a new set of social needs that can be met. It can be achieved only through buoyancy in the work force, and it's a job to do together."

